Transverse Vaginal Septum Cause of Urinary Retention
 Case: L.R., a 15-year-old female, presented to an emergency department with an inability to void for 13 hours, as well as lower abdominal pain. She denied significant past medical history, except anxiety. She denied trauma, sexual activity, menses, and drug use. She had no dysuria, and a urinalysis was negative. A Foley catheter was placed after a bedside bladder scan showed >600ml. She was taught to perform straight catheterization as needed and was discharged with a diagnosis of urinary retention.
Case: L.R., a 15-year-old female, presented to an emergency department with an inability to void for 13 hours, as well as lower abdominal pain. She denied significant past medical history, except anxiety. She denied trauma, sexual activity, menses, and drug use. She had no dysuria, and a urinalysis was negative. A Foley catheter was placed after a bedside bladder scan showed >600ml. She was taught to perform straight catheterization as needed and was discharged with a diagnosis of urinary retention.
Another episode of urinary retention occurred 2 weeks later, while on an airplane, which she attributed to anxiety from flying. She again had similar symptoms a few weeks later. The symptoms resolved each time with catheterization. She then was referred to our pediatric urology practice.
On physical examination, her abdomen was soft and nontender, and the bladder was not palpable. She had normal appearing external female genitalia, her lower back was normal on exam, and she ambulated with a normal gait. A post-void bladder scan demonstrated >400 mL.
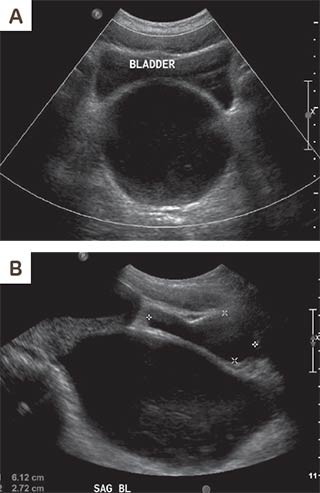
A renal bladder ultrasound and an MRI of her lumbosacral spine were ordered. MRI of the spine was unremarkable for spinal pathology. Ultrasound demonstrated a normal appearing bladder that was compressed by a posterior 14 x 7.5 cm fluid-filled structure. (See Figure 1.)
Discussion: Renal bladder ultrasound demonstrated a normal bladder and normal kidneys without hydronephrosis. A markedly distended debris-filled vagina and mildly distended cervical canal and uterus were noted, along with compression of the urinary bladder. Upon further discussion, the patient noted that the urinary retention seemed to be cyclical over the past several months. She had not experienced visible menstruation. Accumulated menstrual fluid causing significant hydrometrocolpos was causing the patient’s intermittent urinary retention through outflow obstruction.
Differential diagnosis of hydrometrocolpos in an adolescent includes imperforate hymen, transverse vaginal septum (TVS), and distal vaginal atresia. Visible introitus and no visible hymenal bulge made the diagnosis of imperforate hymen less likely. Pelvic MRI (see Figure 2) was performed and demonstrated a severely dilated vagina, mild distention of the uterus, normal appearance of ovaries, presence of a cervix, and low TVS.
Intraoperatively a distal intravaginal bulge was noted, also consistent with TVS. A needle was placed through the septum, and old menstrual blood was noted. Approximately 1 liter of menstrual blood was aspirated from the vagina prior to resection of TVS. Two weeks post-operatively, the patient was healing well and advised to begin using vaginal dilators to help prevent vaginal stenosis. Two months post-operatively, the patient reported having no recurrent episodes of urinary retention, difficulty voiding or pelvic pain and reported having normal menses. The patient was able to place a tampon without issue and exam showed no evidence of vaginal stricture. One year post-operatively the patient continued to have no issues with menses or tampon placement, and exam showed no concern for vaginal stenosis.
TVS are rare: 1 in 70000
TVS are thought to arise from a vertical fusion abnormality of the urogenital sinus and Mullerian ducts during embryologic development, or failure of canalization of the vagina. Estimated incidence of TVS is 1 in 70000 females. TVS can be of varying thickness and can be located in the upper, middle, or lower vagina. Some TVS have a small perforation, which can allow for slow drainage of menstrual fluid. Females with complete TVS typically present with primary amenorrhea and obstructive symptoms of pelvic or lower abdominal discomfort, which is often cyclical. TVS can present with difficulty with urination and defecation due to outflow obstruction, as was the case with this patient, but these are not the most common presenting symptoms.
Imaging modalities that can aid in the diagnosis of TVS are pelvic ultrasound and pelvic MRI. Pelvic MRI can help determine the location Hematocolpos is a typical finding on both pelvic ultrasound and MRI in a patient with TVS who has started to menstruate.
TVS can be surgically corrected by one of several procedures: simple incision, excision, “Z”-plasty, or grafting depending on the location and thickness of the septum.
Watch for post-op vaginal stenosis
The most common complication after resection of TVS is vaginal stenosis. A vaginal mold or vaginal dilation may be recommended after surgery to help prevent post-operative contraction and vaginal stenosis.
There is thought to be an increased risk of retrograde menstruation and subsequent endometriosis with obstructive vaginal lesions such as TVS.
Prompt diagnosis and treatment of obstructive vaginal anomalies helps prevent recurrence of obstructive symptoms and decreases the risk of persistent retrograde menstruation. Although TVS less frequently presents with urinary retention, obstructive vaginal anomalies should be considered in the differential diagnosis for urinary retention in an adolescent female, and as this case illustrates, imaging is paramount in avoiding delay in diagnosis.
References and suggested readings:
Hoffman BL, Schorge JO, Halvorson LM, et al. Williams Gynecology. Fourth ed. New York: McGraw-Hill; 2020. https://accessmedicine.mhmedical.com/book. aspx?bookid=2658. Accessed March 3, 2023.
Partin AW, Dmochowski RR, Kavoussi LR, Peters C. Campbell-Walsh-Wein Urology. Twelfth ed. Philadelphia PA: Elsevier; 2021: 327, 398, 408, 978-980.