Relief from Chronic Pancreatitis Pain: A Case Study
By Petar Mamula, MD, Alexander Y. Coe, MD, MEd, Pablo Laje, MD, & Jefferson N. Brownell, MD
This clinical case study describes a patient with acute recurrent – and then chronic – pancreatitis that was first managed via an endoscopic procedure. The patient’s chronic pain was ultimately relieved by a surgical procedure, a pancreatico-jejunostomy, commonly known as a Puestow procedure.
Background
The patient, a 10-year-old male, was admitted to Children’s Hospital of Philadelphia (CHOP) with abdominal pain and vomiting. He was ultimately diagnosed with pancreatitis. During the patient’s early adolescence, the patient had a series of hospital admissions for acute recurrent pancreatitis and fairly rapidly developed signs of chronic pancreatitis. These admissions had a significant negative impact on the quality of the patient’s life and mental health despite psychological support.
Diagnostic findings
Diagnostic testing included both laboratory tests and imaging.
- Genetic testing revealed variants in two genes associated with pancreatitis: SPINK1 (2 risk allele copies) and CFTR (1 pathogenic copy)
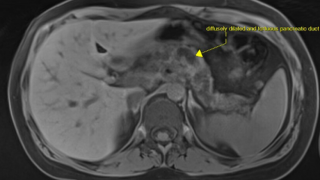
- Magnetic resonance cholangiopancreatography (MRCP) (See Fig. 1) showed abnormalities in the pancreatic ducts including a stricture in the main pancreatic duct with dilation, debris, and stones, as well as dilated side branches. There was also atrophy of the pancreatic parenchyma.
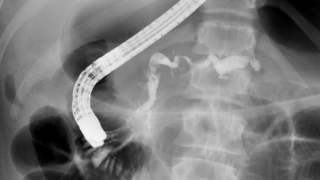
- Endoscopic retrograde cholangiopancreatography (ERCP) was performed to remove the stone in the pancreatic duct. It was notable for similar findings of a dilated and tortuous pancreatic duct and an area of duct narrowing that was dilated. There were also multiple filling defects seen, consistent with stones. These were able to be removed via extraction balloon. A temporary plastic stent was placed, then removed about a month later. A fluoroscopy image (See Fig. 2) from the ERCP demonstrates a widely dilated and tortuous pancreatic duct with a stricture.
Clinical course/treatment
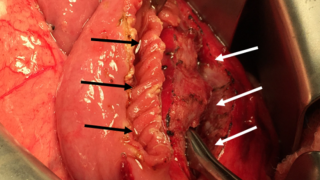
The patient’s symptoms of chronic pain persisted despite successful endoscopic treatment, and we determined he would benefit from a lateral pancreatico-jejunostomy, or Puestow procedure. In this operation, the dilated pancreatic duct was first opened longitudinally as extensively as possible (See white arrows in Fig. 3).
Next, a segment of the small bowel was brought to the upper abdomen in a Roux-en-Y configuration. This segment was opened on the anti-mesenteric side (see black arrows in Fig. 3) for a length that matches the length of the opened pancreatic duct.
Finally, the opened small bowel was anastomosed to the opened pancreatic duct to provide a permanent low-pressure outlet for the pancreatic fluid.
Outcomes
After surgery, the patient did not have any further admissions for pancreatitis. Within a few days of surgery, the patient reported he was pain-free for the first time in a long time. At a follow-up appointment 2-months post-op, the patient reported he was feeling better and experiencing improved sleep.
A year after surgery, the patient continued to be pain-free. He reported being able to have a productive social and academic life. Despite the atrophic appearance of the pancreas, the patient has not had any evidence of exocrine pancreatic insufficiency and has not required pancreatic enzyme replacement therapy to-date. He will continue to be monitored annually.
Discussion
Patients with chronic pancreatitis have a wide spectrum of symptomatology that may change as the disease progresses. In this patient’s case, the presence of multiple genetic risks and pathogenic variants known to be associated with chronic pancreatitis likely contributed to an aggressive and rapid progression of his disease.
Despite endoscopic removal of obstructing stones and dilation of the stenotic segment of the pancreatic duct, recurrent admissions and chronic pain persisted. This led to a multidisciplinary consensus that the lateral pancreatic-jejunostomy would be the best option for further therapeutic intervention.
The resolution of recurrent episodes of pancreatitis and chronic pain highlight the benefit that surgical decompression procedures can have for patients with large duct chronic pancreatitis. Working with the family to address the specific features of the patient’s pancreatic disease allows for a tailored and evidence-based approach to ultimately provide the best outcomes.
Specialists at CHOP’s Pancreatic Disorders Program provide comprehensive, multidisciplinary care for children with acute, recurrent, and chronic pancreatitis, as well as evaluation and management of digestive/exocrine pancreatic insufficiency and its consequences. Surveillance for immediate, short term and long term sequalae are part of the care we provide.
Our team provides the spectrum of care necessary for the proper diagnosis and management of patients with pancreatic disorders. CHOP provides a wide breadth and depth of non-invasive imaging capabilities, endoscopic function testing, ERCP, endoscopic ultrasound, and surgical options including duct decompression procedures like the lateral pancreatico-jejunostomy for large-duct disease and total pancreatectomy with islet auto-transplantation (TPIAT) for small-duct disease.
Our program is one of only a few pediatric centers in the nation accredited by the National Pancreas Foundation (NPF) as both a Center for Clinical Excellence and Academic Excellence for the treatment of pediatric pancreatitis. Key collaborations with other departments at CHOP –and with industry leaders like the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN), the International Study Group of Pediatric Pancreatitis: In Search for a CuRE (INSPPIRE), the NPF, and Mission: Cure – allow us to share our experience and build upon the latest research to help more pediatric patients with pancreatic disorders.
Petar Mamula, MD, is a pediatric gastroenterologist and Director of the Kohl’s Nutrition and Diagnostic Center at Children’s Hospital of Philadelphia. He has special expertise in treating children with pancreatic disorders. Alexander Y. Coe, MD, MEd, is a fellow with the Division of Gastroenterology, Hepatology and Nutrition at CHOP. Pablo Laje, MD, is an attending surgeon in the Division of General, Thoracic and Fetal Surgery. Jefferson N. Brownell, MD, is an attending physician in the Division of Gastroenterology, Hepatology and Nutrition. This article was reviewed by Asim Maqbool, MD, Director of CHOP’s Pancreatic Disorders Program.